9 things you need to know about Borrelia miyamotoi 02/18/2013
Posted by thetickthatbitme in Diagnosis, Media, TBID Facts.Tags: Borrelia, Borrelia hermsii, Borrelia miyamotoi, health, Lyme Disease, medicine, New England Journal of Medicine, Relapsing Fever, tick bite, tick-borne relapsing fever
4 comments
Several months ago, when the patient support group that I attend first began discussing Borrelia miyamotoi, a Google search (or Bing…whatever…) for those two odd words yeilded very little. Now, after the publishing of a few key papers in the New England Journal of Medicine, every major news outlet seems to be aware of this “new” Borrelia.
From a scientific perspective, Borrelia miyamotoi is interesting because it challenges a dichotomy that was established by researchers of tick-borne infectious diseases. When I first started reading about the Borrelia genus, I learned that Borrelia species could be sorted into two major categories: the Lyme disease-like group and the relapsing fever group. That is, Borrelia species like B. burgdorferi, B. afzelli, and B. garinii–which are genetically more similar, are carried by hard-bodied ticks, and cause the same pattern of symptoms (rash, joint pain, fatigue–were put in one group. Other species, like B. hermsii and B. parkeri–which differ genetically from these Lyme-like bacteria, are carried by soft-bodied ticks, and all cause relapsing fever symptoms–were put in the other group. One group for Lyme-like illness. Another group for relapsing fever-like illness. One group for hard-bodied ticks. Another group for soft-bodied ticks. The dichotomy is so clear that the ticks are sometimes referred to as “Lyme disease ticks” and “relapsing fever ticks.”
The funny thing about dichotomies is that they only create the illusion of two distinct categories. The reality is far more messy and characterized by shades of grey. Enter Borrelia miyamotoi. According to its genetics, it should go in the relapsing fever group, but it’s transmitted by the same hard-bodied ticks that carry Lyme disease. According to its symptoms, it falls somewhere in the middle. About 10% of people get a rash, like with Lyme disease, while others don’t. Some people get relapsing fevers, while others don’t. It’s all so very confusing!
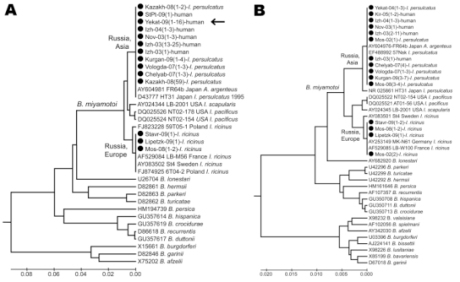
A Borrelia family tree (technically called a phylogenetic tree) highlighting strains of B. miyamotoi. Note the groupings of the other Borrelia. Via Platonov AE, Karan LS, Kolyasnikova NM, Makhneva NA, Toporkova MG, et al. (2011) Humans infected with relapsing fever spirochete Borrelia miyamotoi, Russia. Emerg Infect Dis 17: 1816–1823.
As usual, both the researchers and the news media seem to be trying to downplay this. Some are unwittingly obscuring the issue altogether. “Paging Dr. House: There [sic] a new tick-transmitted spirochete in town…” writes Melissa Healey of the L.A. Times. “The New England Journal of Medicine on Thursday published two reports documenting its arrival on U.S. shores.” As if the bacteria hopped on a boat from Russia, and that’s how it got here! Forget the strong possibility that it was here all along and our scientists just failed to detect it. Forget the possibility that the countless numbers of people who tested negative for Lyme disease and were denied treatment could in fact have this similar infection.
Dr. Peter Krause, lead author on the NEJM study, says (in a video for Yale News) he doesn’t think people should panic about Borrelia miyamotoi. At the same time, he admits that this is an infection that is affecting people in both the eastern and western United States–not to mention people in Europe and Asia. “We expect this disease to be found everywhere the deer tick is found,” he states. So don’t panic, but it’s everywhere.
Okay, so Dr. Krause is right when he says people shouldn’t panic, but that doesn’t mean that we shouldn’t learn more about this new–or not so new, as the case may be–infection, especially since many of us could have it right now. Here are nine things I think you should know about Borrelia miyamotoi.
1. Symptoms: Borrelia miyamotoi causes symptoms of tick-borne relapsing fever (TBRF), an illness often misdiagnosed as Lyme disease, or not diagnosed at all. Tick-borne relapsing fever, when left untreated, has some symptom overlap with Lyme: arthralgias, myalgias, chronic fatigue, and cognitive problems; however, it differs from Lyme disease in that most patients with TBRF get repeated episodes of fever, and they don’t get erythema chronicum migrans (EM), the “classic Lyme” bull’s-eye rash. We can guess that the long-term effects of B. miyamotoi infection are similar to those of other Borrelia infections, even if researchers are reluctant to admit it. Dr. Peter Krause, one of the authors of the study published in the January 17 issue of the New England Journal of Medicine, told the L.A. Times: “This is a very new disease, but none of the patients have had this long-term [neurological] trouble or other long-term symptoms,[…] it’s possible that we just haven’t seen it yet.” Long-term neurological problems from a disease that most doctors didn’t know existed until a few months ago? I’d say it’s very possible.
2. Transmission: Borrelia miyamotoi is transmitted to humans from the bites of hard-bodied ticks. Examples of these ticks include Ixodes scapularis (deer tick), Ixodes pacificus (western blacklegged tick), Ixodes ricinus (castor bean tick), and Ixodes persulcatus (taiga tick). (The first two tick species listed are common in North America, and the second two are found in Europe and Asia.)
3. Why you’re just hearing about it now: The B. miyamotoi bacterium was discovered in ticks and mice in Japan back in 1995. (It’s named after Japanese entomologist Kenji Miyamoto, who first isolated the bacterium.) In 2001, Dr. Durland Fish discovered B. miyamotoi in ticks in Connecticut, but according to a 2011 New York Times report, he “was repeatedly refused a study grant [from NIH] until the Russians proved it caused illness.” In 2011, Russian scientists, in collaboration with the Yale team that included Krause and Fish, published research that showed that B. miyamotoi infects humans. The patients in the 2011 study were in Russia, so B. miyamotoi didn’t really come on the radar for U.S. doctors until January 2013, when a study on U.S. patients was published by Krause and colleagues in the New England Journal of Medicine.
4. Testing: To my knowledge, there is currently no commercially-available test for B. miyamotoi, be it PCR, IFA, or Western Blot. B. miyamotoi has been detected using assays (tests) that were developed by university researchers in order to study the bacterium. That means, unless your doctor is at Yale or another large institution, it’s not likely that he or she has access to a test for B. miyamotoi. So if you suspect you may be infected, what can you do? That brings me to my next point.
5. People with B. miyamotoi infection are likely to test negative for B. burgdorferi (Lyme disease), unless they also happen to be infected with B. burgdorferi. Doctors who are only screening patients for Lyme disease are not going to catch all of the other Borrelia infections, like B. miyamotoi.
6. Genetically, B. miyamotoi is more similar to other bacteria that cause TBRF, like Borrelia hermsii. Therefore, people with B. miyamotoi infection may test positive for B. hermsii, another relapsing fever spirochete.
7. As with any infection, B. miyamotoi infection can be more serious in the elderly and in patients with compromised immune systems. If you or a family member is denied treatment, especially in the case of severe or life-threatening symptoms (like high fever), my advice would be to go to a tertiary care center (like a university hospital) and ask to be tested for B. miyamotoi. At the very least, doctors at a research hospital should be able to do a blood smear to look for spirochetes (Borrelia). PCR and antibody tests may also be available.
8.Treatment: B. miyamotoi probably responds in a similar way to antibiotics as other Borrelia like B. hermsii and B. burgdorferi. Researchers claim that it can be treated with a few weeks of oral antibiotics, but that is probably only for mild, acute cases. My guess (as a non-medical-professional) is that B. miyamotoi is just as resilient as its Borrelia cousins and requires 4-6 weeks of daily IV antibiotics. If you’re new to this blog, you might be interested in reading about my experience being treated with IV antibiotics for B. hermsii (relapsing fever).
9. Recommended reading: To learn more about B. miyamotoi, check out the new fact sheet, which includes links to peer-reviewed studies.
Related articles
Reactive Arthritis and the Chronic Lyme Disease Debate: Dissecting the Research 11/20/2012
Posted by thetickthatbitme in Diagnosis, Peer-Reviewed, Tick-Lit, Treatment.Tags: antigens, Arthritis, Borrelia, Chronic Lyme disease, health, Infectious Diseases Society of America, joints, Journal of Clinical Investigation, Lyme, Lyme Disease, medicine, mouse, research, spirochete, steroids, Yale
7 comments
As you may be aware, there is a great deal of controversy about persistence of Lyme disease symptoms after treatment—even when treatment involves long-term antibiotics. There are many theories about this, and several of them may be true, depending on the patient. The Centers for Disease Control (CDC) and the Infectious Diseases Society of America (IDSA) say that once you’ve been treated with a month of antibiotics, you no longer have a Borrelia burgdorferi infection. If you’re still experiencing symptoms, they call it Post-Lyme or antibiotic-refractory arthritis. At the other end of the spectrum, some Lyme-literate medical doctors (LLMDs) believe that Lyme is a chronic disease, and once you have it, you’ll have it for life. Long-term (read: indefinite) antibiotic treatment, they maintain, is necessary to keep the organisms from multiplying, but you’ll never fully be rid of them.
My views fall somewhere between these two extremes. (Disclaimer: I am not a medical professional.) On the one hand, I don’t think that four weeks of antibiotics, whether oral or intravenous, is really enough to kill off a Borrelia infection in a patient who’s been infected for years. (And this view is supported by Embers et al’s study of Rhesus macaques.) On the other hand, I don’t think that antibiotics-for-life is the answer either. There are just too many people who have been on antibiotics for years who don’t seem to be getting better. Plus there’s the fact that antibiotics can cause a lot of damage if you take them long-term, which significantly lowers the quality of life for people on these treatment regimens.
So when patients have been treated and they’re still experiencing symptoms, I see several possible explanations:
1) The antibiotics didn’t kill off all the bacteria, and they are still hanging around somewhere—perhaps hidden in joints, cartilage, or the brain. This, as you can imagine, is very difficult to prove, especially in living human beings.
2) The antibiotics killed off all the bacteria, but the patient was bitten by another tick and re-infected. This is highly possible if the patient’s environment, lifestyle, and preventive measures have not changed. It’s also difficult to detect when patients are only being follow-up tested with Western Blots, and not something like the C6 antibody assay, which gives you a titer so you can see if your antibodies to the bacteria suddenly increase. (A study related to reinfection was just published on Wednesday in the New England Journal of Medicine. You can read about it in the NY Times here, or read the study abstract. I’ll be doing a run-down of that study next week.)
3) The antibiotics killed off the bacteria, but the body is still making an immune response, possibly attacking its own cells, causing inflammation and continuing symptoms.
When new research comes out, I like to pay attention to see which of these explanations is supported and why. In this post, I’ll take you through a study called “Spirochete antigens persist near cartilage after murine Lyme borreliosis therapy” that was conducted by some researchers at Yale and published in the Journal of Clinical Investigation back in June. (If you want to read along, you can access the full article here.)
Some Background:
The underlying question in this study is: what causes Lyme-associated arthritis in patients who have been treated with antibiotics? Is it that infectious spirochetes are still hiding somewhere in the body, or is it possible that antibiotics “kill” all the bacteria (read: disassemble them so they can’t multiply) but leave their building blocks (referred to as antigens because the body still detects them) behind, causing inflammation.
Let me explain how killing Borrelia in the human body works. The things you need to kill Borrelia are antibodies, first and foremost. If you don’t generate an IgM response, this infection can be fatal in the first 3 to 7 days. We know that IgM has a direct bactericidal effect. In other words, this antibody can kill Borrelia on its own in the absence of complement. IgG, by comparison, is very inefficient at killing Borrelia, but we make that, too. We also need phagocytes to kill Borrelia, and in order to generate antibodies, we need B cells that work. Another thing we need is toll-like receptors (TLRs). These are important for helping antibodies bind to pathogens or parts of pathogens. If we’re deficient in TLR2, or a certain molecule in TLR called myeloid differentiation antigen 88 (abbreviated MyD88), we can have an overwhelming infection.
What they did:
In this study, the researchers used a type of mouse in which this MyD88 protein has been knocked out—i.e. the mouse is totally deficient in MyD88. For that reason, they call it a Myd88-/- mouse. (No, that thing at the end is not an emoticon.) The problem with these mice is that they die quickly of opportunistic infection (specifically, Pneumocystis carinii), so in the lab, they have to give them an antibiotic called Sulfatrim or Septra, which is actually a combination of two antibiotics—sulfamethoxazole and trimethoprim. I’ll come back to why this is important a little later.
Now, an interesting thing is that this same group of researchers did a study back in 2002 using C3H mice, who don’t have the Myd88 protein knocked out—so essentially “normal” mice, in terms of their immune systems—and they showed that live Borrelia persist for 3 months after optimal treatment. These Borrelia that remained were sort of mutant Borrelia because they were missing a couple of proteins that they might need to infect other animals. The researchers knew this because the clean ticks that bit them got B. burgdorferi, but when they had those ticks bite healthy mice, those mice didn’t get infected.
Anyway, for some reason, these researchers didn’t want to use the C3H mice for this study, and they decided to use the Myd88-/- mice, who develop overwhelming infections. They also used a WT strain of mouse (which is not missing Myd88) for the sake of comparison. They infected both types of mice, and then they treated some of them with Doxycycline (through their water supply) and others with Ceftriaxone (via subcutaneous injection). Interestingly, they showed that after one day of Ceftriaxone therapy, they could kill all of the Borrelia. They also used an interesting microscopic technique which allows one to look real-time at tissue and watch an organism to see what it does. By cutting down to a mouse’s tendon, they can see what’s going on down there.
Their Findings:
“B. burgdorferi DNA can be detected in B6 Myd88-/-, but not WT, mice after treatment with Doxycycline” (p. 2).
Translation: After treating the mice with Doxycycline, the researchers couldn’t find any B. burgdorferi DNA in the normal immune system mice, but they could find the DNA in the immune-compromised mice. One of those mice had a positive culture for B. burgdorferi, and ticks that fed on that mouse also tested positive for B. burgdorferi. HOWEVER, when they took samples from the knee joints of the mice, ALL of the mice tested positive for the ospA plasmid (B. burgdorferi DNA). In addition, ear-skin samples from half the immune-compromised mice and one of the normal mice tested positive for B. burgdorferi DNA (p. 2).
“Real-time imaging of B. burgdorferi in Myd88-/- mice reveals rapid spirochete elimination after antibiotic therapy” (p. 2).
Translation: The researchers used intravital 2-photon microscopy to observe the behavior of the B. burgdorferi spirochetes in the infected mice. Specifically, they looked at the dermis (skin) and the calcaneal (achilles) tendons. They say that 24 hours after beginning treatment with Ceftriaxone, the number of spirochetes had “diminished dramatically” in both the skin and tendons. The spirochetes left behind in the skin appeared to be moving, but the ones in the tendons did not. The following day, they were not able to see any spirochetes using this imaging technique, suggesting that they had all been destroyed.
“Spirochete antigens can be detected adjacent to ear cartilage in antibiotic treated Myd88-/- mice” (p. 3).
Translation: At the end of the study, the researchers took tissue samples from the ears of all the mice. They tested these samples for B. burgdorferi using both immunofluorescence staining (looking for antibodies) and culture techniques. The mice who were “sham treated” (not given antibiotics) tested positive. The mice who were treated with Ceftriaxone had negative cultures, but some “spirochete antigens” were detected in a deep layer of skin next to the ear cartilage. By “spirochete antigens,” they mean not live spirochetes but proteins (building blocks) left over from the bacteria that can cause the immune system to react. These antigens were found at a deeper level than where the imaging had earlier been peformed (which explains why they weren’t detected using imaging). The same antigens were detected in ear tissue from mice treated with Doxycycline. The researchers conclude that because the antigens were detected, but the bacteria could not be cultured (grown), it means whatever these spirochete remains were, they were incapable of multiplying because they had been too damaged by the antibiotics.
“Live imaging reveals antigen deposits but not motile spirochetes adjacent to cartilage of Myd88-/- mice after Doxycycline treatment for B. burgdorferi infection” (p. 3).
Translation: A separate experiment was conducted in which researchers studied mice between 2 and 10 weeks after finishing a 1 month course of Doxycycline. They used a technique called xenodiagnosis, where they let clean ticks bite the mice. They could find some B. burgdorferi DNA in the ticks that fed on the mice treated with Doxycycline, but when they studied the contents of the ticks’ guts, they could not find any spirochetes. By contrast, the ticks that fed on mice not treated with antibiotics had the bacteria in their bellies. In addition to using xenodiagnosis, they did the immunofluorescence test and cultures on this group of mice, and as before the cultures were negative and the immunofluorescence found antigens near the ear cartilage. This time, they used their imaging technique to look deeper under the skin, closer to the ear cartilage. In the sham treated mice, they found that there were motile (alive) spirochetes right next to the cartilage and large “deposits of nonmotile fluorescent material” where the skin meets the cartilage. In the antibiotic-treated mice, they saw no live spirochetes, but the same deposits were present next to the cartilage. So to see if these deposits would cause infection, the researchers transplanted skin from the infected mice (both those treated with Doxycycline and the sham-treated ones) into non-infected mice. Only the skin from sham-treated mice caused infection in the new mice. This shows that the antigens adjacent to ear cartilage in the mice treated with Doxycycline were not infectious.
“Spirochete antigens can be detected in joints of antibiotic-treated C3H Myd88-/- mice” (p. 4).
Translation: Here, the researchers decided to look at the knee joints of the mice to see if the same antigen deposits exist in antibiotic-treated mice. They looked at the knees of mice that had been infected for 4 months (which is a long time considering mice only live for about a year). When they treated these mice with Ceftriaxone, intravital microscopy showed that the spirochetes died off, but debris was left behind. They are pretty sure the spirochetes died off because the cultures were negative.
“Tissues from antibiotic-treated mice contain immunogenic and inflammatory B. burgdorferi antigens” (p. 4).
Translation: Finally, they wanted to test whether the deposits left behind in the knees of the mice actually contained B. burgdorferi antigens. They did this by immunizing new mice with knee tissue from the infected mice. They found that both the tissue from sham-treated and antibiotic-treated mice caused an IgG immune response to several B. burgdorferi proteins in the new mice.
Problems with the study:
1. It’s in mice. If you follow the research on B. burgdorferi, you’ll see that many of the studies are done in mice. That’s because it’s much less expensive to study disease in mice than in other animals. However, if we really want to learn about arthritis and B. burgdorferi in the human body, it would be better to do a study like this in Rhesus monkeys, which are much more similar to humans. Hopefully, this study will make it possible for some researchers to try to replicate this work in a primate model so that we can learn more.
2. The use of a “lab” strain of B. burgdorferi. They used a 297 strain of Borrelia burgdorferi which is “stable”–in other words, it’s not changing. It’s old and predictable. The problem is that most Borrelia in the wild are likely mutating and changing. They could even be developing resistance to antibiotics. After all, these organisms have been around for thousands of years; they are masters of adaptation. It would be much more interesting to do a study like this using a “wild” strain of B. burgdorferi, as this would more closely mimic the average patient’s experience.
3. The ambiguous blot analysis. The researchers used their own immunoblot to look at the antigens in the patellas (knees) of the mice. It’s not clear to me why they didn’t just use a Western Blot (since that’s the test used on us humans). Another odd thing they did was use a dilution of 1:1,000 for the blot, which is ten times the dilution used for other blots. Perhaps a lower dilution showed too many similarities between the sham group and the antibiotic group? In any case, for a study like this, I would expect more justification for these unusual choices.
4. The study’s “lack of heart” (and brain). I’m referring to the fact that the researchers failed to examine the effect of B. burgdorferi in the hearts of the mice. We know that, in addition to knee problems, patients with B. burgdorferi infections are at risk for a variety of heart problems, including myocarditis. The researchers were so bent on showing that antibiotics could kill the bacteria near joints, but what does that matter if the heart is still infected? If they truly believe that 24 hours of Ceftriaxone in mice eliminates B. burgdorferi, they missed a golden opportunity to show it by neglecting to examine the hearts–and the brains, for that matter. Not only did they ignore the heart, but they wasted valuable word space in their discussion section attacking the research design of Embers et al’s 2012 study of B. burgdorferi infection in Rhesus macaques. Now, the infamous monkey study is far from perfect, but they did do one thing right, which was to look at the heart tissue of the monkeys post-mortem–and guess what they found? In 3 out of 12 monkeys who were treated with antibiotics (that’s 25%), B. burgdorferi RNA could be detected in the heart. That’s despite the fact that in all 12 of the treated animals, C6 antibody titers decreased steadily over the course of treatment.
5. The use of septra/Sulfatrim. This one is a doozy. Earlier, I mentioned that the researchers added the antibiotic sulfamethoxazole-trimethoprim (Sulfatrim) to the mice’s drinking water “to reduce opportunistic infection”(p. 7). They claim that this drug has “no effect on B. burgdorferi infection or disease”(p. 7). I’m guessing they think that because of this 1996 study done in Austria. In that study, several species of Borrelia were evaluated to see whether they were susceptible to amoxicillin, azithromycin, cefotaxime, ceftriaxone, doxycycline, penicillin G sodium, roxithromycin, and trimethoprim-sulfamethoxazole (Sulfatrim) in vitro. The researchers used 30 different strains of Borrelia, but only 4 of those were Borrelia burgdorferi, and they were European B. burgdorferi at that. They found that B. burgdorferi was resistant to trimethoprim-sulfamethoxazole. Now, even though both ceftriaxone and trimethoprim-sulfamethoxazole were studied, the Austrian researchers didn’t investigate what would happen if you used both of these drugs on the Borrelia at the same time (which is what was done in the Yale study). In fact, after scouring PubMed, I was unable to find any synergistic Borrelia studies using ceftriaxone and trimethoprim-sulfamethoxazole. I did, however, find this study, also from Austria, published in 1997. They found that “trimethoprim was more active against Borrelia burgdorferi than against a sensitive strain of Escherichia coli, but sulfamethoxazole was not active against Borrelia burgdorferi.” In other words, one of the drugs that makes up Sulfatrim kills Borrelia, and the other doesn’t. The question is, if you add Ceftriaxone, does Sulfatrim start killing the Borrelia? To actually know whether or not Sulfatrim has an effect on B. burgdorferi when combined with Ceftriaxone, our Yale researchers would have had to do a synergy study, to see what would happen if you took the 50% kill rate of Doxycycline and Ceftriaxone, and add Sulfatrim. But they didn’t show that adding Sulfatrim didn’t affect the kill. So when they’re saying that “Ceftriaxone rapidly [within 24 hours] reduces pathogen burden in the skin,”(p. 5) they’re not taking into account that the Sulfatrim in the drinking water is also probably helping kill off spirochetes. It’s ironic how critical they are of other studies when their own study isn’t exactly “clean.”
6. The way Doxycycline was administered. Doxycycline was given to the mice in their drinking water. This means that the amount of Doxycycline in each mouse’s system depended on how much water it drank. The researchers said their reason for doing the Doxy in the water instead of force-feeding it to the mice twice a day was that when it was given twice daily, serum drug levels fell too low and they were not able to kill all the bacteria (p. 5). When I read this, I thought to myself, “Well, let’s see, how many humans do I know who are taking their Doxycycline through their drinking water? Oh, that’s right. None.” So here we have a study of Borrelia burgdorferi infection in mice in which the researchers choose not to give oral antibiotics because they believe not that the drug doesn’t work, but that the drug delivery system doesn’t work because it can’t get a high enough level of the drug into the blood stream. Yet, these are the same doctors who are saying that one month of oral Doxycycline should be enough to treat the same infection in humans. Curious, isn’t it? They even admit that one mouse may have stayed sick “due to a drinking pattern that led to inconsistent Doxycycline levels” (p. 5). So I guess either that mouse just wasn’t as thirsty as all the other mice, or he was eating his food and drinking his water in one sitting, and the food interfered with the drug absorption (as it can in people!).
7. They didn’t treat the arthritis. Okay, I get that the researchers were having lots of fun with their innovative real-time imaging technique. They tried to accomplish a lot with this study, and it already appears that they may have spread themselves a little thin. However, it bothers me that they spent no time examining ways to treat the arthritis caused by the deposits left behind by B. burgdorferi. In the world outside the laboratory, it doesn’t so much matter to people whether their arthritis is caused by live spirochetes or dead ones. They want to know what’s going to make them feel better. The study’s authors suggest that more antibiotics likely won’t work, but they don’t explore any alternatives, like steroids, for treating Lyme arthritis.
Some interesting (and some unexpected) implications:
1. Cool pictures. Intravital microscopy, the real-time imaging technology used in this study, is pretty nifty, and could be used in better-designed studies to find out a lot of useful information. The researchers in this study could even see some of the spirochetes changing into spherical forms, but they didn’t really investigate or discuss this in detail, beyond saying they don’t think those forms are bacterial cysts. It might be useful to have an entire study dedicated to investigating that.
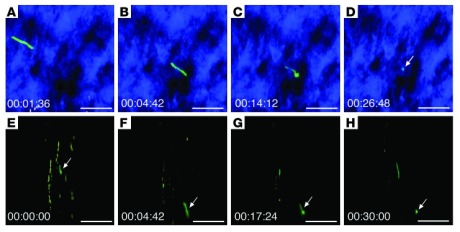
Image sequences of Bb914 (Borrelia burgdorferi) changing from an elongated spirochete to a spherical form. (Image via ncbi.nlm.nih.gov; J Clin Invest. 2012 July 2; 122(7): 2652–2660.)
2. Rethinking oral Doxycycline. It’s been my belief for a while now that oral antibiotics are just not as effective at killing Borrelia as IV antibiotics like Ceftriaxone. I’m not expecting everyone to agree with me on this, but let me tell you why I think so. While Doxycycline is by far the best choice among oral antibiotics for killing Borrelia (as it’s better at crossing the blood-brain barrier than many other drugs), there is an inherent disadvantage to all oral drugs because they have to be delivered through our digestive system. As a patient who took Doxy for a month, I can tell you that no matter how responsible and organized you are, it is very difficult to eat meals at the same time every day, to space the doses 12 hours apart, and to avoid ingesting things like milk that interfere with drug absorption. Reading Bockenstedt et al’s article made me further question the effectiveness of oral Doxy, as the researchers decided that oral Doxy twice per day would not be enough to keep serum drug levels consistent. Instead, they opted to deliver the drug through the mice’s water supply, which poses other problems with consistency. In any case, if it’s not good enough for lab mice, I don’t see how it’s good enough for humans.
3. A new drug combo? The study shows that in the presence of trimethoprim, you can rapidly kill Borrelia with Ceftriaxone. That means we should be doing more studies on how this works and whether it is safe for humans. There is always concern with killing off bacteria too rapidly because macrophages need time to clear the debris (which we think causes arthritis). However, this drug combination seems worth examining in other laboratory studies.
4. Location, location, location. The study doesn’t show that cartilage can be infected with Borrelia burgdorferi, but it does show that deposits are left over near cartilage after the bacteria have been disassembled by antibiotics. If the infection is in cartilage, that’s bad news, because there is no blood flow to cartilage, so it’s very difficult to eradicate an infection there. We need more studies that examine how this bacterium acts around cartilage.
5. Chronic Lyme? Contrary to what Yale alum and journalist Carole Bass would have you believe (Thanks to Becki from Bloody Lymey for opening my eyes to that one.), this study neither proves nor disproves the existence of Chronic Lyme disease, so despite the agenda that may underlie this study, patients need not see it as a threat. The study authors themselves admit in their Discussion section that they’re not quite sure what all their data mean: “The significance of B. burgdorferi DNA in xenodiagnostic ticks and in mouse tissues after antibiotic therapy is unclear” (p. 5). One possibility is that “Some B. burgdorferi DNA could remain intact if it is sequestered in cellular debris such as the GFP deposits.” They’re saying they think that the B. burgdorferi DNA they detected is just remnants of dead spirochetes that were preserved because they were stuck in the debris left behind by the antibiotics. However, they also admit to another possibility: “Alternatively, spirochete DNA could represent a minor subpopulation of B. burgdorferi that is not killed by the antibiotic treatment.” It’s a one-sentence admission in a 9-page paper, but it’s there–and it means that despite what these researchers think is going on, they still can’t say with 100% certainty that the antibiotics completely eradicated the infection.
What the study does show is that there are deposits in mouse tissue that the researchers insinuate are dead organisms (they have Borrelia antigens, are immunogenic, and don’t appear to be infectious). Because they don’t examine all of the tissue–including the cartilage, the heart, and the brain–it’s difficult to say whether they have completely eliminated the bacteria with antibiotics. What Embers et al showed in their primate model is that there seems to be persistence of spirochetes following 4 weeks of IV Ceftriaxone treatment and 8 weeks of Doxycycline. Until somebody does another study in Rhesus monkeys and proves that they’re wrong, that study stands.
6. Treating the arthritis. We know that reactive arthritis caused by Borrelia infections is a real phenomenon, and this study suggests that the cause is the debris left behind by spirochetes following antibiotic treatment. However, what patients and doctors alike need is access to information about how best to treat this unique form of arthritis. I’ve heard anecdotes from patients and doctors about the helpfulness of steroids like prednisone during or following antibiotic treatment, but there really isn’t enough research being done on this. It would be nice if researchers on both sides of the Chronic Lyme debate would pool their resources for the sake of better patient care.
I hope you enjoyed this installment of Tick-Lit Tuesday. It’s good to be back.
What has been your experience with Lyme or Tick-borne Relapsing Fever and reactive arthritis? What questions would you like to see addressed in future research?
Related articles
Six Tick Misconceptions 07/05/2012
Posted by thetickthatbitme in Diagnosis, Prevention, TBI Facts.Tags: Babesia, Borrelia, Colorado Tick Fever, health, Lyme Disease, medicine, misconception, Ornithodoros, prevention, Rickettsiosis, Rocky Mountain Spotted Fever, tick, Tick-borne disease
4 comments
I have a confession to make. I have a phobia of most creepy-crawly things–roaches, mosquitoes, spiders, and especially ticks. When I see pictures of any of these critters, my first instinct is to shield my eyes. Ick! But what I should be doing is taking notice, so that if a tick ever gets on me again, maybe I can identify that little jerk.
Today’s post is about the misconceptions that many people have about ticks. As I warn frequently, there’s a lot of misinformation about ticks and the diseases they spread in the mainstream media and on the Internet. Here are six big misconceptions.
#1: Only deer ticks transmit diseases.
Deer ticks (a.k.a. blacklegged ticks) carry a lot of pathogens, including those that cause Lyme disease, Anaplasmosis, Babesiosis, and Bartonellosis, but they’re not the only ones you need to worry about. Dog ticks (Dermacentor variabilis) and wood ticks (Dermacentor andersoni) carry Rocky Mountain spotted fever (Rickettsiosis), Tularemia, and the Colorado Tick Fever virus. The lone star tick (Ambylomma americanum) carries Ehrlichiosis and the pathogen that causes STARI; bites from this tick have also been linked to a delayed allergic reaction to red meat. Two other types of Rickettsiosis, Rickettsia parkeri and 364D Rickettsiosis can be transmitted by the Gulf Coast tick (Amblyomma maculatum) and the Pacific Coast tick (Dermacentor occidentalis), respectively. Q fever (Coxiella burnetii) can be transmitted by the brown dog tick (Rhipicephalus sanguineus), Rocky Mountain wood tick (Dermacentor andersoni), and the lone star tick (Amblyomma americanum). Last but not least, soft-bodied ticks like Ornithodoros hermsi, Ornithodoros parkeri, and Ornithodoros turicata transmit Relapsing Fever-causing species of Borrelia. These ticks can live up to ten years!
#2: Lyme disease is the most dangerous thing I can get from a tick.
Though life-threatening complications like myocarditis can occur in the later stages of Lyme disease, B. burgdorferi infection is rarely fatal in the first months of infection. Many patients survive years without being properly diagnosed and treated. By contrast, Rickettsiosis (Rocky Mountain spotted fever) can be fatal in the first 8 days of symptoms (which vary greatly from person to person and don’t always involve the spotted rash) if it goes untreated. Female tick saliva also contains a neurotoxin that can cause tick paralysis, which can be fatal if the tick is not found and removed.
#3: I can’t get sick unless the tick is attached 36-48 hours.
While the CDC claims this is true for Lyme disease, if the tick has bitten you, there’s always a chance that bacteria or a virus is already in your system. Even if the tick doesn’t infect you with bacteria or a virus, you are still at risk for tick paralysis (see #2). In the case of soft-bodied Ornithodoros ticks, which spread Relapsing Fever Borrelia, feeding may only take a few minutes, and then the tick falls off, often undetected. (You can read more about soft-bodied ticks here.)
#4: If I don’t go hiking or camping, I’m not going to get bitten by a tick.
While participation in these activities does put you at higher risk for tick exposure, ticks can hide out in plenty of other places besides the forest floor, including the leaf litter in your yard. Ticks can hitch a ride into your yard on any of the wildlife on which they feed, including deer, mice, squirrels, and birds. They can hitch a ride into your house on your dog or cat. And don’t forget other four-legged friends like horses and sheep. If you have mice in your house or attic, you probably also have ticks. To avoid exposure, you should limit your contact with leaf litter, tall grasses, wood piles, and bird feeders. When hiking, stay in the middle of trails, wear long pants tucked into your socks, and wear repellent. Avoid sleeping in cabins that may be infested with rodents (and thereby ticks). After spending time outdoors or with animals, do a thorough tick-check. (This requires getting naked.) And if you’re a fan of spelunking, know that ticks—particularly soft-bodied ones—can live in caves too.
#5: If I don’t have a rash or a fever, the tick that bit me didn’t give me a disease.
At least 20% of people infected with Borrelia burgdorferi (Lyme) don’t have the characteristic erythema chronicum migrans (bull’s-eye) rash (EM). People with other tick-borne illnesses may be asymptomatic or have other symptoms (like joint and muscle pain or fatigue) that may not directly suggest an infection. That’s why it’s important to keep track of all of your symptoms following a tick bite, and to save the tick for identification and testing. You should always make sure your doctor is aware of any tick bites or tick exposures you may have had—and be clear about what regions/countries you’ve visited and what animal exposure you’ve had.
#6: I can use soap or Vaseline to remove a tick, and afterwards I should burn it with a match.
The proper way to remove a tick is with tweezers, grabbing the tick close to the skin, and using a slow, steady motion to pull it out. Using soap or Vaseline will not help you get a better grip on the tick, and may increase the likelihood that you squeeze the tick, causing it to regurgitate bacteria and other pathogens into your skin. Once you remove the tick, you should store it in a secure container and bring it to your doctor’s office for identification and testing. If you do get sick, it will be helpful to know what kind of tick it is and what pathogens it’s carrying. Don’t destroy the evidence with a match! If for some reason you can’t save the tick (because you’re too busy spelunking), at the very least try to take a picture of it. You’ll probably need a zoom lens.
So how do I spot them?
I usually try to link to pictures of ticks instead of posting them on this site because seeing tick photos can be a bit traumatizing to those of us who have been sick with tick-borne infections. However, for the purpose of prevention education, I’ve included pictures of all the ticks mentioned in this post (that I could find) in the slideshow below. You can read about the geographic distribution of hard-bodied ticks in the U.S. here and the habitats of soft-bodied ticks here.
Related articles
Major Misnomer: 8 things you need to know about Rocky Mountain spotted fever 06/05/2012
Posted by thetickthatbitme in Diagnosis, TBI Facts, Treatment.Tags: Arizona, CDC, coinfection, dogs, doxycycline, fatality, Lyme Disease, medicine, rash, Rickettsia, Rocky Mountain Spotted Fever, tick, transfusion
3 comments
The fact sheet for Rocky Mountain spotted fever (Rickettsia) is up today. Here’s the cliff notes version:
1. You don’t have to be in the Rocky Mountains to catch RMSF. There are four types of ticks in the U.S. that can transmit this bacteria to you: the American dog tick (Dermacentor variabilis), Rocky Mountain wood tick (Dermacentor andersoni), brown dog tick (Rhipicephalus sanguineus), and the Cayenne tick (Amblyomma cajennense). Cases of RMSF have been reported all over the U.S., and there have also been some in Canada. In 2008, all but 8 states reported cases of RMSF to the CDC.
2. Rocky Mountain spotted fever can be a deadly disease if not treated promptly. The national fatality rate is about 3%, but this rate is much higher in certain states like Arizona, where the fatality rate is 10%. This is likely due to delayed diagnosis.
3. Patients infected with the Rickettsia rickettsii bacteria that causes RMSF may experience any combination of the following symptoms: chills, confusion, fever, headache, muscle pain, rash, diarrhea, light sensitivity, hallucinations, loss of appetite, nausea, thirst, and vomiting. Though 90% of patients develop the spotted rash, this often comes late in the illness, so if other symptoms are present, you shouldn’t wait to get treated. Ten percent of patients never develop the rash.
4. RMSF can be diagnosed with a blood antibody test called an IFA (indirect immunofluorescence assay), but this test is often negative in the first week or so of infection. If you are showing symptoms of RMSF, your doctor shouldn’t wait for blood test results before putting you on antibiotics, because the longer treatment is delayed, the higher the risk of fatality.
5. RMSF is treated with Doxycycline in both adults and children. The usual course is between 7 and 14 days. The CDC recommends treating for at least 3 days after fever subsides.
6. Another way to get RMSF is by squashing ticks that you find on your dog (or anywhere else) with your bare fingers. When you squish a tick, the bacteria inside it can come out and enter your body through your skin. When checking your pets for ticks, always wear gloves, and use tweezers for tick removal.
7. Although very rare, it is possible to get RMSF from a blood transfusion. If you experience symptoms of RMSF following a transfusion, see your doctor right away.
8. The symptoms of RMSF can mimic those of other TBIDs, like Ehrlichiosis and Anaplasmosis. Luckily, all three of these are treated with Doxycycline.
If you want to read more about RMSF, check out the fact sheet, which is full of links to additional information.
Related articles
Ehrlichia: confusing cousins, the blood supply, and the new kid on the block 05/04/2012
Posted by thetickthatbitme in Diagnosis, TBI Facts.Tags: Blood donation, Blood transfusion, CDC, Ehrlichia, health, Lyme Disease, medicine, Minnesota, Rocky Mountain Spotted Fever, tick, Wisconsin
5 comments
Ehrlichia…I just met a girl named Ehrlichia…and suddenly the sound…
Nope. Doesn’t quite work.
Ehrlichia is actually named after German microbiologist Paul Ehrlich (1854-1915), who won the Nobel Prize in 1908. Here are some things you actually need to know about Ehrlichia:
1. Ehrlichia is transmitted through the bites of lonestar ticks and deer ticks. If you’ve had another infection carried by these ticks (like Lyme Disease), your doctor should have had you tested for Ehrlichia (or maybe you’ll be asking him/her to test you after reading this post?).
2. Symptoms of Ehrlichiosis include: fever, headache, chills, malaise, muscle pain, nausea / vomiting / diarrhea, confusion, conjunctival injection (red eyes), and rash (in up to 60% of children, less than 30% of adults). When it goes untreated (or improperly treated), complications can include breathing problems, bleeding disorders, and death (1.8% of cases).
3. Ehrlichia is effectively treated with doxycycline in both adults and children. The CDC recommends a 7-14 day course.
4. Your doctor shouldn’t wait for your test results to come back before prescribing you doxycycline. If your doctor thinks you might have Ehrlichiosis, he/she might order a PCR, a blood smear, or an IFA (antibody test). These tests can take a few weeks to come back, and in that time, you could get very, very sick. In addition, a negative result on any of these three tests does not rule out the possibility of infection. Often, in the first 7-10 days you are infected, you will test negative. For more information about these tests, take a look at the Ehrlichiosis fact sheet.
5. Ehrlichia can be easily misdiagnosed as one of two other infections. It’s a rickettisial disease, which means it’s in the same family with A. phagocytophilum and Rocky Mountain Spotted Fever (RMSF). Sometimes the rash patients get with Ehrlichia looks a lot like the rash patients get with RMSF.
6. It may be possible to contract an Ehrlichia infection through a blood transfusion. The CDC has not been very vocal about it, but it’s on their website. Fun fact: “Ehrlichia chaffeensis has been shown to survive for more than a week in refrigerated blood.” If you’ve had an Ehrlichia infection, it’s probably not a good idea for you to be a blood or organ donor.
7. There’s a newly identified species of Ehrlichia in Wisconsin and Minnesota. It doesn’t have a fancy species name yet, so scientists refer to it as Ehrlichia Wisconsin HM543746 or Ehrlichia muris-like (EML). This one is carried by deer ticks. If you live in one of these states and your doctor is not so hip to the new infectious disease research, he or she may have told you that you didn’t need to be tested for Ehrlichia because “we don’t have that here.” (I hate it when doctors say that!)Hopefully there will be a commercially-available, species-specific test for this soon. For now, my guess is that physicians in Wisconsin and Minnesota who suspect Ehrlichia infection are ordering tests for E. chaffeensis and E. ewingii.
Got an Ehrlichia story you’d like to share? Shoot me an e-mail.
Related articles
Well, Babs, you’re trickier than I thought 05/01/2012
Posted by thetickthatbitme in Diagnosis, Peer-Reviewed, TBI Facts, Tick-Lit.Tags: Babesia, Blood donation, Blood transfusion, health, IFA, labs, Lyme, medicine, PCR, smear, tick
1 comment so far
Welcome to the second installment of Tick-Lit Tuesday, where I comb through PubMed so you don’t have to. Today’s topic: Babesia and Blood Transfusions. Now, I know I posted about Babesia in the blood supply just a few days ago, but an interesting study has since come to my attention (thanks, Dr. W), and the implications are a bit scary. Okay, get your popcorn and let’s begin.
The Issue:
It has been well-documented that the tick-borne protozoan parasite Babesia can be contracted through blood transfusions. Blood centers aren’t required to test donated blood for Babesia, but this may change in the future, as Babesia infections contracted through transfusions are on the rise. So if we were to test all donors for Babesia prior to donation, which tests should we rely on to detect this pesky parasite? Let’s look at the candidates.
IFA: IFA is an abbreviation for indirect fluorescent antibody test. This type of test can also be referred to as serologic (as in blood serum) testing. If you’ve had one of these tests for Babesia, it’s probably titled something like “WA1 IGG ANTIBODY IFA” (for B. duncani) or “BABESIA MICROTI ABS IGG/IGM” on your lab results. If you’ve had Babesia in the past and been treated for it, your antibody test might still read positive because your body is still making antibodies to the parasite. This is one of the reasons why most insurance companies refuse to pay for treatment for Babesia if your only positive test is the IFA. They think maybe you had a past infection that you got over, so you don’t need treatment. (The other reason they refuse to pay is that they’re jerks, to put it nicely.) I’ll talk more about why this is such a problem later in this post.

A stained blood smear on which B. microti parasites are visible in red blood cells. (CDC Photo: DPDx). Via CDC.gov.
Smear: When we talk about a smear for Babesia, we mean a Giemsa-stained thin blood smear. This test involves looking at blood samples under a microscope to see if there are any parasites hanging around. The problem with this test is that Babesia can infect fewer than 1% of your circulating red blood cells, so it could take many, many smears before any Babesia show up under the microscope. For more information about that phenomenon, read this.
PCR: This stands for polymerase chain reaction. It’s basically a DNA test that tries to identify whether a gene associated with Babesia is present in the blood. PCR has been found to be “as sensitive and specific” as blood smears for Babesia (see this study), which is not saying much, considering the tendency of Babesia to go undetected with smears.
Hmmm, for whom shall I cast my ballot, the antibody test insurance companies don’t trust, the inaccurate smear, or the inaccurate PCR? Choices, choices…
Today’s question:
Can the donated blood of someone with a negative PCR and negative blood smear still be infected with Babesia and cause Babesia infection in transfusion recipients?
(Hint: This is a leading question.)
Let’s talk about a study published in the journal Transfusion in December of 2011 called “The third described case of transfusion-transmitted Babesia duncani.”
Here’s what happened:
In May 2008, a 59 year-old California resident (I’ll call him Cal) with sickle-cell disease had some red blood cell transfusions. Cal’s only risk factor for Babesia was the transfusions; he didn’t have any tick exposure. In September of 2008, Cal was diagnosed with a Babesia duncani (WA-1) infection. The parasites were visible on a blood smear, the indirect fluorescent antibody (IFA) test was positive, and the PCR was positive for the Babesia gene. This launched a transfusion investigation in which doctors tracked down 34 of the 38 blood donors whose blood could have infected Cal with Babesia. One donor, a 67-year-old California resident (who I’ll call Don) had a B. duncani titer of 1:4096 (on the IFA test). What does a titer of 1:4096 mean? Well, if the antibody test for B. duncani is negative, the titer will be < 1:256. That means that Don’s antibody test was positive.
What the article abstract doesn’t tell you, which the full article does, is that both Don’s PCR and blood smear were negative for Babesia. How did the researchers prove definitively that Don had Babesia in his blood? They injected the blood into Mongolian gerbils, and were later able to isolate the parasite from the gerbils. Conclusion: Even though Don showed no symptoms of Babesia and both his PCR and smear were negative, his donated blood caused Babesiosis in both Cal and the gerbils.
Here’s why the study’s findings are important:
1. Clearly, blood smears and PCRs are not good indicators of whether someone is infected with Babesia. Why insurance companies think these tests need to be positive before they’ll pay for treatment is a mystery to me. There are probably a lot of people out there who’ve had positive IFAs but negative smear and/or PCR who were then not treated for Babesia because either the doctor, the insurance company, or both said they didn’t have an infection.
2. As far as the blood donation goes, if we don’t start screening out donors with positive Babesia IFAs, we’re going to continue to contaminate the blood supply with Babesia. It should be as simple as that. Been bitten by a tick? No blood donation for you. Positive IFA? No blood donation for you.
DZWSQK6QYS9G
Related articles
Eight things you need to know about Anaplasmosis 04/25/2012
Posted by thetickthatbitme in Diagnosis, TBI Facts.Tags: Anaplasma phagocytophilum, Anaplasmosis, Borrelia burgdorferi, doxycycline, health, labs, Lyme Disease, medicine, Rocky Mountain Spotted Fever, tick, treatment
5 comments
A new fact sheet is up today for Anaplasmosis, otherwise known as Anaplasma phagocytophilum infection. Try saying that three times fast. This is one of the two TBIDs I’ve been unlucky enough to have, but I had never heard of it before my lab results came back with a positive antibody test for it. By the end of this post, you’ll know eight things you didn’t know before about Anaplasmosis.
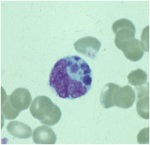
A microcolony of A. phagocytophylum visible in a granulocyte (white blood cell) on a peripheral blood smear. Image via CDC.gov.
1. Anaplasmosis is spread by the same ticks that spread Borrelia burgdorferi (Lyme Disease). This means that people with Lyme can have a coinfection with Anaplasmosis (and some of them don’t know it).
2. The symptoms of an Anaplasma phagocytophilum infection are: fever, headache, muscle pain, malaise, chills, nausea / abdominal pain, cough, and confusion. Some people get all the symptoms; other people only get a few.
3. If you show symptoms of Anaplasmosis, your doctor shouldn’t wait for lab results to come back to begin treating you. The CDC recommends beginning treatment right away.
4. If you’ve been infected with Anaplasma phagocytophilum and you get tested within the first 7-10 days you are sick, the test might come back negative. This doesn’t mean you don’t have Anaplasmosis, and you’ll need to be tested again later.
5. The best way to treat Anaplasmosis is with the antibiotic Doxycycline. According to the CDC, other antibiotics should not be substituted because they increase the risk of fatality. If your doctor insists on treating your Anaplasmosis with something other than Doxycycline, it’s probably time to get a new doctor. For people with severe allergies to Doxycycline or for women who are pregnant, the drug Rifampin can be used to treat Anaplasmosis.
6. Anaplasmosis can be confused with other TBIDs in the rickettsia family like Rocky Mountain Spotted Fever (RMSF) and ehrlichiosis. These infections are also commonly treated with Doxycycline.
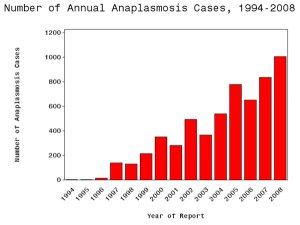
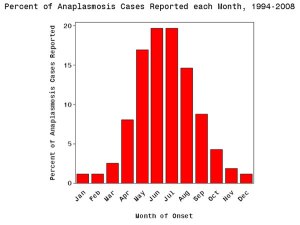
7. The number of cases of Anaplasmosis reported to the CDC has increased steadily since 1996. You can attribute this to climate change or not, but the trend suggests that this disease will be an increasingly more common problem in the future.
8. More than half of Anaplasmosis cases are reported in the spring and summer months. This is a no-brainer, since this is when tick populations thrive. To avoid infection, take steps to avoid tick exposure for both you and your pets.