5 Things That Helped Me Heal 05/02/2012
Posted by thetickthatbitme in Humor, Whole Person.Tags: Arthritis Foundation, Craig Ferguson, exercise, Geoff Peterson, healing, health, Heating pad, humor, Memory foam, treatment
3 comments
1. Shower chair
We got this after I had my back surgery (to help me avoid bending, slipping, and falling), and I continued to use it after I was diagnosed with hermsii and Anaplasmosis. It really makes a difference being able to sit and relax while bathing. My boyfriend (who is healthy as a horse) also enjoys using it when he just wants to wash his feet!
2. Thermalon heating pads
These heating pads are my best friends. My mom, who has Arthritis, introduced me to them. I put mine in the microwave for about a minute, and it will stay warm for about 30, depending on how cold my house is. After the initial heating, you can reheat them for 30-40 seconds at a time. I prefer these to an electric heating pad because they provide moist heat, and I can fall asleep with one without burning myself. They helped me get off painkillers and sleep better on cold nights. They can also double as cold packs if you store them in the freezer inside a ziplock bag. I found them on sale at Walgreens for $15 each.
3. Low-impact exercise
Taking an Arthritis Foundation water aerobics class at a warm water therapy pool helped me stay active while I was getting treated. The warm water helped my joints feel better, and I think all the endorphins from exercising made me happier. I also made some great friends in the class who are just slightly older and much wiser than me. (Shout out to the pool ladies!) If you’re interested in this type of class, you can search for one in your area here.
4. Memory foam mattress pad
This was also a purchase made after my back surgery. My mattress is quite firm. (That’s how I used to like it when I was a young thing with no health problems.) I’ve always slept best on my side, but after surgery, and as I began developing more joint problems in my neck, hips, and knees, the mattress was too hard for me. Rather than shelling out $800 for a new mattress, I spent about $150 for this memory foam mattress topper from Costco. Now the bed is soft enough that I don’t feel like I’m sleeping on a plank, but not so soft that I sink in too far. I’m still able to roll over during the night so I don’t get too stiff.
5. Geoff Peterson
I can’t stress enough how much laughter helped me recover. My parents are a little obsessed with Craig Ferguson, and I started watching him, too, when I was staying with them and getting IV therapy. Craig’s exchanges with his robot sidekick Geoff Peterson make me laugh the hardest.
What are some things that have helped your healing process?
Eight things you need to know about Anaplasmosis 04/25/2012
Posted by thetickthatbitme in Diagnosis, TBI Facts.Tags: Anaplasma phagocytophilum, Anaplasmosis, Borrelia burgdorferi, doxycycline, health, labs, Lyme Disease, medicine, Rocky Mountain Spotted Fever, tick, treatment
5 comments
A new fact sheet is up today for Anaplasmosis, otherwise known as Anaplasma phagocytophilum infection. Try saying that three times fast. This is one of the two TBIDs I’ve been unlucky enough to have, but I had never heard of it before my lab results came back with a positive antibody test for it. By the end of this post, you’ll know eight things you didn’t know before about Anaplasmosis.
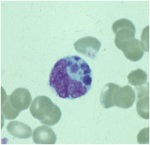
A microcolony of A. phagocytophylum visible in a granulocyte (white blood cell) on a peripheral blood smear. Image via CDC.gov.
1. Anaplasmosis is spread by the same ticks that spread Borrelia burgdorferi (Lyme Disease). This means that people with Lyme can have a coinfection with Anaplasmosis (and some of them don’t know it).
2. The symptoms of an Anaplasma phagocytophilum infection are: fever, headache, muscle pain, malaise, chills, nausea / abdominal pain, cough, and confusion. Some people get all the symptoms; other people only get a few.
3. If you show symptoms of Anaplasmosis, your doctor shouldn’t wait for lab results to come back to begin treating you. The CDC recommends beginning treatment right away.
4. If you’ve been infected with Anaplasma phagocytophilum and you get tested within the first 7-10 days you are sick, the test might come back negative. This doesn’t mean you don’t have Anaplasmosis, and you’ll need to be tested again later.
5. The best way to treat Anaplasmosis is with the antibiotic Doxycycline. According to the CDC, other antibiotics should not be substituted because they increase the risk of fatality. If your doctor insists on treating your Anaplasmosis with something other than Doxycycline, it’s probably time to get a new doctor. For people with severe allergies to Doxycycline or for women who are pregnant, the drug Rifampin can be used to treat Anaplasmosis.
6. Anaplasmosis can be confused with other TBIDs in the rickettsia family like Rocky Mountain Spotted Fever (RMSF) and ehrlichiosis. These infections are also commonly treated with Doxycycline.
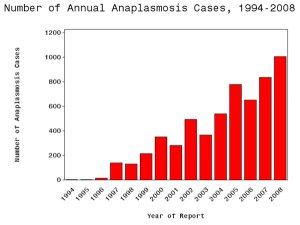
7. The number of cases of Anaplasmosis reported to the CDC has increased steadily since 1996. You can attribute this to climate change or not, but the trend suggests that this disease will be an increasingly more common problem in the future.
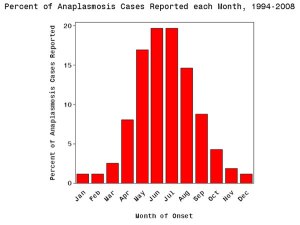
8. More than half of Anaplasmosis cases are reported in the spring and summer months. This is a no-brainer, since this is when tick populations thrive. To avoid infection, take steps to avoid tick exposure for both you and your pets.
What Is Prophylaxis, and Does It Work on Tick Bites? 04/24/2012
Posted by thetickthatbitme in Peer-Reviewed, Tick-Lit, Treatment.Tags: Borrelia burgdorferi, Borrelia hermsii, Borrelia persica, CDC, doxycycline, health, Israel, Lyme Disease, medicine, NEJM, prevention, prophylaxis, research, TBRF, tick bite, treatment
3 comments
Today is Tuesday, and I’ve made an executive decision that from now on, every Tuesday I will be covering peer-reviewed research related to tick-borne infections. We in academia call this a “review of the literature,” even though it’s not what normal people think of as literature–no Shakespeare, just dry prose littered with scientific jargon–which is why most people don’t want to read it. Lucky for you, I am a super-nerd and enjoy this kind of reading, at least when it’s about TBIDs (tick-borne infectious diseases). I’ve even come up with an affectionate name for it: “tick-lit”. So every Tuesday from here on out will be Tick-Lit Tuesday, the day on which I read the literature so you don’t have to. Enjoy!
Today’s question: Does prophylaxis work for tick bites?
While a lot of patients with tick-borne infections don’t remember a tick or a tick bite (which is why it takes so long to get diagnosed), there are also people who do notice being bitten and go to a doctor right away because they are concerned about TBIDs. So what happens to these patients?
I’ve heard stories from patients with TBIDs, particularly patients with Borrelia burgdorferi (Lyme) and Borrelia hermsii (Tick-borne Relapsing Fever), about how when they went to a doctor within 48 hours of being bitten, they were told “Oh, we don’t have Lyme in this state, so you don’t have to worry.” Following this logic, ticks carrying Borrelia burgdorferi must be so smart that 1) they know which bacteria they are carrying; 2) they know which state they are in; and 3) they have the decency to respect state lines. I can really imagine a deer tick saying, “Oh, no, I can’t go over there. I’m a California tick. They don’t let dirty ticks like me out of California.” I suppose some doctors imagine that there is some kind of tick parole system that keeps them from traveling anywhere where the CDC and state health departments have not documented them to exist.
Some of these delusional doctors probably can’t be reasoned with, but what about doctors who want to do the right thing? What should they do when a patient comes to them within 48 hours of a tick bite?
Let’s take a look at the research.
One of my favorite tick-lit studies is one that was published in the New England Journal of Medicine way back in July 2006. The study took place in Israel, where Ornithodoros tholozani ticks infect people with a bacterium called Borrelia persica. Borrelia persica, like Borrelia hermsii, causes Tick Borne Relapsing Fever (TBRF). You can think of Borrelia persica as B. hermsii‘s brother. The researchers wanted to find out whether prophylaxing soldiers (giving them antibiotics right away) who had recently been bitten by ticks would prevent the infection from spreading and causing the symptoms of TBRF.
Here’s how they did it (Methods). They studied 93 healthy soldiers with suspected tick bites. Some of these people had evidence of a tick bite (like a rash) and others didn’t, but had been in the same places that the people with bites had, so they had the same risk of exposure. They randomly picked half of the soldiers who would receive antibiotics (Doxycycline for 5 days), and the other half would receive a placebo (which means they would think that they were taking antibiotics, but they were really taking a sugar pill). The study was double-blind, which means that neither the soldiers nor the researchers knew which patients were given the real antibiotics at the time of the study. This makes the study more credible.
Here’s what happened (Results):
All 10 cases of TBRF identified by a positive blood smear were in the placebo group of subjects with signs of a tick bite (P<0.001). These findings suggested a 100 percent efficacy of preemptive treatment (95 percent confidence interval, 46 to 100 percent). PCR for the borrelia glpQ gene was negative at baseline for all subjects and subsequently positive in all subjects with fever and a positive blood smear. Seroconversion was detected in eight of nine cases of TBRF. PCR and serum samples were negative for all of the other subjects tested. No major treatment-associated adverse effects were identified.
In English, this means that 10 of the 46 people who did not get treated with antibiotics got sick with TBRF, and their blood tests showed that they were making antibodies to Borrelia persica. (Their PCR test (a DNA test) was also positive for the borrelia gene.) However, none of the 47 people who were treated with antibiotics developed any symptoms of TBRF. When their blood was tested, it was negative for antibodies to Borrelia persica and their PCR was negative for the borrelia gene. That means that prophylaxing with Doxycycline prevented 100% of cases of TBRF (Borrelia perica infection).
- Doxycycline Structure. Image via Wikipedia.
- Doxycycline 3D structure. Image via Wikipedia.
Now you may say to yourself, “Oh, that’s only one study. The sample size was fairly small, and it’s not necessarily generalizable to all Borrelia infections.” At least, that’s what I imagined you (or your skeptical primary doctor) saying as I was rooting around on PubMed. Then I dug up this study from *gasp* 2001: “Prophylaxis with single-dose doxycycline for the prevention of Lyme disease after an Ixodes scapularis tick bite” (!!!)
The 2001 study was conducted in an area of New York with a high incidence of Borrelia burgdorferi (Lyme) infection. Like the Israeli study, it was also a randomized, double-blind, placebo-controlled trial, but unlike the Israeli study, they only gave patients a single dose of doxycycline. The results? One out of the 235 people treated with doxycycline got Erythema migrans, the bull’s-eye rash that indicates a Borrelia burgdorferi infection. In the placebo group (people who didn’t get antibiotics) 8 out of 235 developed the rash and tested positive for infection. Their conclusion: a single dose of doxycycline can prevent Lyme if given within 72 hours of the tick bite.
If these two studies are not convincing or current enough, the doctors from the Israeli Medical Corps published another study in 2010. First, they inform us that “Since 2004, the Israel Defence Forces (IDF) has mandated the prophylaxis of tick-bitten subjects with a five-day doxycycline course.” (That has me thinking the Israelis are pretty smart.) Just to make sure they were doing the right thing, in this study, they decided to analyze all the tick bite and TBRF cases in their records from 2004-2007.
Here’s what they say:
Of those screened, 128 (15.7%) had tick-bite and were intended for prophylaxis, of which four TBRF cases occurred-3.13% attack rate compared with an expected rate of 38.4% in these bitten individuals without prophylaxis (RR = 0.08, number needed to treat = 3). In all cases in which screening and prophylaxis were provided within 48 h of tick bite, complete prevention of TBRF was achieved. No cases of Jarisch-Herxheimer reaction (JHR) was recorded.
What does that mean? Only 4 of the 128 people who were treated with doxycycline developed TBRF, a rate of 3.13%. The expected attack rate was more than 10 times that, 38 percent, so without the doxycycline policy, it would likely have been 48 people with TBRF instead of 4. One more thing. There was a reason those four people got sick: they were given the doxycycline later than 48 hours after being bitten!
The Big Picture
How does this research affect you as a patient who has been bitten by a tick and contracted an infection or as a patient who could potentially be bitten by a tick in the future?
The research shows us that, if treated within 48 hours with 5 days of Doxycycline, most–if not all–cases of Borrelia infection and resulting symptoms can be prevented. If you could get an appointment with an infectious disease specialist who recognizes this fact within 48 hours of being bitten, you could probably avoid a lot of potential suffering. The problem is that to see a specialist, you usually need to be referred by your primary care doctor. Some of us can’t even get an appointment to see our primary care doctors within 48 hours, and some of the primary care doctors don’t even know how to spell Borrelia (no offense to primary care doctors who can spell it), let alone diagnose it with a simple blood test. And most of them certainly don’t know that the best thing to do would be to prophylax you with doxycycline.
Let’s put the numbers in perspective. In 2010, the CDC reported over 20,000 confirmed cases of Lyme (Borrelia burgdorferi) and an additional 10,000 probable cases. The CDC’s number of cases (which I believe, as with burgdorferi, are severely underreported) for 1990-2011 for Borrelia hermsii (TBRF) is 483. If 35% of those Borrelia cases had been prevented with prophylaxis, that would mean 10,669 fewer sick people.
So what can you do? Here’s a list of my suggestions:
- If you’ve been diagnosed with a tick-borne illness, make sure that every one of your doctors knows it, even the ones you don’t like and the ones you don’t go to very often. All doctors, not just infectious disease doctors, need to be aware of how prevalent these infections are.
- If you are bitten by a tick, insist that your primary care doctor prophylax you with doxycycline for five days. You can even print out these PubMed article abstracts and bring them to your appointment. Many doctors can be reasoned with, and if they won’t listen to you, sometimes they’ll listen to the New England Journal of Medicine.
- If you are bitten by a tick, try your best to save the little beast. You can store it in an old prescription bottle or a jar. (Labs like Quest Diagnostics also distribute collection containers to some doctors’ offices.) Inform your doctor that you are brining the tick to your appointment and you want to have it tested. Having ticks tested helps with more accurate CDC reporting about which areas have infected ticks.
- Getting the tick tested doesn’t mean that you don’t need to get tested. The tick testing takes longer than the people testing. On the off-chance that prophylaxis doesn’t work for you, you’ll need to get more treatment if you test positive.
- As always, the best way not to get a tick bite is not to be in areas where ticks live and not to be around animals that carry ticks. Follow tick-exposure prevention best practices. This includes keeping your home and yard free of mice and rats (on which the hermsii-carrying ticks feed) as well as deer (on which the burgdorferi-carying ticks feed).
That’s all for Tick-Lit Tuesday. Stay informed and stay well!
Curious about Tick-borne Infections? 04/21/2012
Posted by thetickthatbitme in TBI Facts.Tags: Borrelia burgdorferi, Borrelia hermsii, diagnosis, facts, infection, Lyme, Lyme Disease, TBI, tick-borne, treatment, ugly stepsister
2 comments
Happy Saturday, loyal readers!
I thought I’d point out that I’ve added a new section to the blog: Infection Fact Sheets. One of my goals with this blog is to give you, my readers, access to as much factual information about tick-borne infectious diseases–or TBIDs, as I like to abbreviate them–as possible.
Since you’ve stumbled upon this blog, I’m sure you’ve heard of Lyme Disease, but do you know the name of the bacterium that causes it? Are you familiar with the common and not-so-common symptoms? What about the different drugs that are used to treat this infection? Check out the fact sheet here.
And let’s not forget Borrelia hermsii, which I consider to be like Lyme’s neglected ugly stepsister. Nope, no press for Ms. B. hermsii… Take pity on her (or if not her, me, a hermsii survivor) and pay a visit to her fact sheet.
If I were truly going to put my teacher hat on and plan a lesson for you, I’d tell you to make a K-W-L chart and take notes!
Once you’re done with the Borrelia sisters, you’ll probably be hungering (or worrying?) for more TBID info. Here’s a list of what’s to come: Anaplasmosis, Babesiosis (WA-1), Ehrlichiosis, Rickettsia (Rocky Mountain Spotted Fever), and more!