Six Tick Misconceptions 07/05/2012
Posted by thetickthatbitme in Diagnosis, Prevention, TBI Facts.Tags: Babesia, Borrelia, Colorado Tick Fever, health, Lyme Disease, medicine, misconception, Ornithodoros, prevention, Rickettsiosis, Rocky Mountain Spotted Fever, tick, Tick-borne disease
4 comments
I have a confession to make. I have a phobia of most creepy-crawly things–roaches, mosquitoes, spiders, and especially ticks. When I see pictures of any of these critters, my first instinct is to shield my eyes. Ick! But what I should be doing is taking notice, so that if a tick ever gets on me again, maybe I can identify that little jerk.
Today’s post is about the misconceptions that many people have about ticks. As I warn frequently, there’s a lot of misinformation about ticks and the diseases they spread in the mainstream media and on the Internet. Here are six big misconceptions.
#1: Only deer ticks transmit diseases.
Deer ticks (a.k.a. blacklegged ticks) carry a lot of pathogens, including those that cause Lyme disease, Anaplasmosis, Babesiosis, and Bartonellosis, but they’re not the only ones you need to worry about. Dog ticks (Dermacentor variabilis) and wood ticks (Dermacentor andersoni) carry Rocky Mountain spotted fever (Rickettsiosis), Tularemia, and the Colorado Tick Fever virus. The lone star tick (Ambylomma americanum) carries Ehrlichiosis and the pathogen that causes STARI; bites from this tick have also been linked to a delayed allergic reaction to red meat. Two other types of Rickettsiosis, Rickettsia parkeri and 364D Rickettsiosis can be transmitted by the Gulf Coast tick (Amblyomma maculatum) and the Pacific Coast tick (Dermacentor occidentalis), respectively. Q fever (Coxiella burnetii) can be transmitted by the brown dog tick (Rhipicephalus sanguineus), Rocky Mountain wood tick (Dermacentor andersoni), and the lone star tick (Amblyomma americanum). Last but not least, soft-bodied ticks like Ornithodoros hermsi, Ornithodoros parkeri, and Ornithodoros turicata transmit Relapsing Fever-causing species of Borrelia. These ticks can live up to ten years!
#2: Lyme disease is the most dangerous thing I can get from a tick.
Though life-threatening complications like myocarditis can occur in the later stages of Lyme disease, B. burgdorferi infection is rarely fatal in the first months of infection. Many patients survive years without being properly diagnosed and treated. By contrast, Rickettsiosis (Rocky Mountain spotted fever) can be fatal in the first 8 days of symptoms (which vary greatly from person to person and don’t always involve the spotted rash) if it goes untreated. Female tick saliva also contains a neurotoxin that can cause tick paralysis, which can be fatal if the tick is not found and removed.
#3: I can’t get sick unless the tick is attached 36-48 hours.
While the CDC claims this is true for Lyme disease, if the tick has bitten you, there’s always a chance that bacteria or a virus is already in your system. Even if the tick doesn’t infect you with bacteria or a virus, you are still at risk for tick paralysis (see #2). In the case of soft-bodied Ornithodoros ticks, which spread Relapsing Fever Borrelia, feeding may only take a few minutes, and then the tick falls off, often undetected. (You can read more about soft-bodied ticks here.)
#4: If I don’t go hiking or camping, I’m not going to get bitten by a tick.
While participation in these activities does put you at higher risk for tick exposure, ticks can hide out in plenty of other places besides the forest floor, including the leaf litter in your yard. Ticks can hitch a ride into your yard on any of the wildlife on which they feed, including deer, mice, squirrels, and birds. They can hitch a ride into your house on your dog or cat. And don’t forget other four-legged friends like horses and sheep. If you have mice in your house or attic, you probably also have ticks. To avoid exposure, you should limit your contact with leaf litter, tall grasses, wood piles, and bird feeders. When hiking, stay in the middle of trails, wear long pants tucked into your socks, and wear repellent. Avoid sleeping in cabins that may be infested with rodents (and thereby ticks). After spending time outdoors or with animals, do a thorough tick-check. (This requires getting naked.) And if you’re a fan of spelunking, know that ticks—particularly soft-bodied ones—can live in caves too.
#5: If I don’t have a rash or a fever, the tick that bit me didn’t give me a disease.
At least 20% of people infected with Borrelia burgdorferi (Lyme) don’t have the characteristic erythema chronicum migrans (bull’s-eye) rash (EM). People with other tick-borne illnesses may be asymptomatic or have other symptoms (like joint and muscle pain or fatigue) that may not directly suggest an infection. That’s why it’s important to keep track of all of your symptoms following a tick bite, and to save the tick for identification and testing. You should always make sure your doctor is aware of any tick bites or tick exposures you may have had—and be clear about what regions/countries you’ve visited and what animal exposure you’ve had.
#6: I can use soap or Vaseline to remove a tick, and afterwards I should burn it with a match.
The proper way to remove a tick is with tweezers, grabbing the tick close to the skin, and using a slow, steady motion to pull it out. Using soap or Vaseline will not help you get a better grip on the tick, and may increase the likelihood that you squeeze the tick, causing it to regurgitate bacteria and other pathogens into your skin. Once you remove the tick, you should store it in a secure container and bring it to your doctor’s office for identification and testing. If you do get sick, it will be helpful to know what kind of tick it is and what pathogens it’s carrying. Don’t destroy the evidence with a match! If for some reason you can’t save the tick (because you’re too busy spelunking), at the very least try to take a picture of it. You’ll probably need a zoom lens.
So how do I spot them?
I usually try to link to pictures of ticks instead of posting them on this site because seeing tick photos can be a bit traumatizing to those of us who have been sick with tick-borne infections. However, for the purpose of prevention education, I’ve included pictures of all the ticks mentioned in this post (that I could find) in the slideshow below. You can read about the geographic distribution of hard-bodied ticks in the U.S. here and the habitats of soft-bodied ticks here.
Related articles
Major Misnomer: 8 things you need to know about Rocky Mountain spotted fever 06/05/2012
Posted by thetickthatbitme in Diagnosis, TBI Facts, Treatment.Tags: Arizona, CDC, coinfection, dogs, doxycycline, fatality, Lyme Disease, medicine, rash, Rickettsia, Rocky Mountain Spotted Fever, tick, transfusion
3 comments
The fact sheet for Rocky Mountain spotted fever (Rickettsia) is up today. Here’s the cliff notes version:
1. You don’t have to be in the Rocky Mountains to catch RMSF. There are four types of ticks in the U.S. that can transmit this bacteria to you: the American dog tick (Dermacentor variabilis), Rocky Mountain wood tick (Dermacentor andersoni), brown dog tick (Rhipicephalus sanguineus), and the Cayenne tick (Amblyomma cajennense). Cases of RMSF have been reported all over the U.S., and there have also been some in Canada. In 2008, all but 8 states reported cases of RMSF to the CDC.
2. Rocky Mountain spotted fever can be a deadly disease if not treated promptly. The national fatality rate is about 3%, but this rate is much higher in certain states like Arizona, where the fatality rate is 10%. This is likely due to delayed diagnosis.
3. Patients infected with the Rickettsia rickettsii bacteria that causes RMSF may experience any combination of the following symptoms: chills, confusion, fever, headache, muscle pain, rash, diarrhea, light sensitivity, hallucinations, loss of appetite, nausea, thirst, and vomiting. Though 90% of patients develop the spotted rash, this often comes late in the illness, so if other symptoms are present, you shouldn’t wait to get treated. Ten percent of patients never develop the rash.
4. RMSF can be diagnosed with a blood antibody test called an IFA (indirect immunofluorescence assay), but this test is often negative in the first week or so of infection. If you are showing symptoms of RMSF, your doctor shouldn’t wait for blood test results before putting you on antibiotics, because the longer treatment is delayed, the higher the risk of fatality.
5. RMSF is treated with Doxycycline in both adults and children. The usual course is between 7 and 14 days. The CDC recommends treating for at least 3 days after fever subsides.
6. Another way to get RMSF is by squashing ticks that you find on your dog (or anywhere else) with your bare fingers. When you squish a tick, the bacteria inside it can come out and enter your body through your skin. When checking your pets for ticks, always wear gloves, and use tweezers for tick removal.
7. Although very rare, it is possible to get RMSF from a blood transfusion. If you experience symptoms of RMSF following a transfusion, see your doctor right away.
8. The symptoms of RMSF can mimic those of other TBIDs, like Ehrlichiosis and Anaplasmosis. Luckily, all three of these are treated with Doxycycline.
If you want to read more about RMSF, check out the fact sheet, which is full of links to additional information.
Related articles
Ehrlichia: confusing cousins, the blood supply, and the new kid on the block 05/04/2012
Posted by thetickthatbitme in Diagnosis, TBI Facts.Tags: Blood donation, Blood transfusion, CDC, Ehrlichia, health, Lyme Disease, medicine, Minnesota, Rocky Mountain Spotted Fever, tick, Wisconsin
5 comments
Ehrlichia…I just met a girl named Ehrlichia…and suddenly the sound…
Nope. Doesn’t quite work.
Ehrlichia is actually named after German microbiologist Paul Ehrlich (1854-1915), who won the Nobel Prize in 1908. Here are some things you actually need to know about Ehrlichia:
1. Ehrlichia is transmitted through the bites of lonestar ticks and deer ticks. If you’ve had another infection carried by these ticks (like Lyme Disease), your doctor should have had you tested for Ehrlichia (or maybe you’ll be asking him/her to test you after reading this post?).
2. Symptoms of Ehrlichiosis include: fever, headache, chills, malaise, muscle pain, nausea / vomiting / diarrhea, confusion, conjunctival injection (red eyes), and rash (in up to 60% of children, less than 30% of adults). When it goes untreated (or improperly treated), complications can include breathing problems, bleeding disorders, and death (1.8% of cases).
3. Ehrlichia is effectively treated with doxycycline in both adults and children. The CDC recommends a 7-14 day course.
4. Your doctor shouldn’t wait for your test results to come back before prescribing you doxycycline. If your doctor thinks you might have Ehrlichiosis, he/she might order a PCR, a blood smear, or an IFA (antibody test). These tests can take a few weeks to come back, and in that time, you could get very, very sick. In addition, a negative result on any of these three tests does not rule out the possibility of infection. Often, in the first 7-10 days you are infected, you will test negative. For more information about these tests, take a look at the Ehrlichiosis fact sheet.
5. Ehrlichia can be easily misdiagnosed as one of two other infections. It’s a rickettisial disease, which means it’s in the same family with A. phagocytophilum and Rocky Mountain Spotted Fever (RMSF). Sometimes the rash patients get with Ehrlichia looks a lot like the rash patients get with RMSF.
6. It may be possible to contract an Ehrlichia infection through a blood transfusion. The CDC has not been very vocal about it, but it’s on their website. Fun fact: “Ehrlichia chaffeensis has been shown to survive for more than a week in refrigerated blood.” If you’ve had an Ehrlichia infection, it’s probably not a good idea for you to be a blood or organ donor.
7. There’s a newly identified species of Ehrlichia in Wisconsin and Minnesota. It doesn’t have a fancy species name yet, so scientists refer to it as Ehrlichia Wisconsin HM543746 or Ehrlichia muris-like (EML). This one is carried by deer ticks. If you live in one of these states and your doctor is not so hip to the new infectious disease research, he or she may have told you that you didn’t need to be tested for Ehrlichia because “we don’t have that here.” (I hate it when doctors say that!)Hopefully there will be a commercially-available, species-specific test for this soon. For now, my guess is that physicians in Wisconsin and Minnesota who suspect Ehrlichia infection are ordering tests for E. chaffeensis and E. ewingii.
Got an Ehrlichia story you’d like to share? Shoot me an e-mail.
Related articles
Eight things you need to know about Anaplasmosis 04/25/2012
Posted by thetickthatbitme in Diagnosis, TBI Facts.Tags: Anaplasma phagocytophilum, Anaplasmosis, Borrelia burgdorferi, doxycycline, health, labs, Lyme Disease, medicine, Rocky Mountain Spotted Fever, tick, treatment
5 comments
A new fact sheet is up today for Anaplasmosis, otherwise known as Anaplasma phagocytophilum infection. Try saying that three times fast. This is one of the two TBIDs I’ve been unlucky enough to have, but I had never heard of it before my lab results came back with a positive antibody test for it. By the end of this post, you’ll know eight things you didn’t know before about Anaplasmosis.
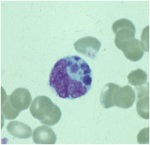
A microcolony of A. phagocytophylum visible in a granulocyte (white blood cell) on a peripheral blood smear. Image via CDC.gov.
1. Anaplasmosis is spread by the same ticks that spread Borrelia burgdorferi (Lyme Disease). This means that people with Lyme can have a coinfection with Anaplasmosis (and some of them don’t know it).
2. The symptoms of an Anaplasma phagocytophilum infection are: fever, headache, muscle pain, malaise, chills, nausea / abdominal pain, cough, and confusion. Some people get all the symptoms; other people only get a few.
3. If you show symptoms of Anaplasmosis, your doctor shouldn’t wait for lab results to come back to begin treating you. The CDC recommends beginning treatment right away.
4. If you’ve been infected with Anaplasma phagocytophilum and you get tested within the first 7-10 days you are sick, the test might come back negative. This doesn’t mean you don’t have Anaplasmosis, and you’ll need to be tested again later.
5. The best way to treat Anaplasmosis is with the antibiotic Doxycycline. According to the CDC, other antibiotics should not be substituted because they increase the risk of fatality. If your doctor insists on treating your Anaplasmosis with something other than Doxycycline, it’s probably time to get a new doctor. For people with severe allergies to Doxycycline or for women who are pregnant, the drug Rifampin can be used to treat Anaplasmosis.
6. Anaplasmosis can be confused with other TBIDs in the rickettsia family like Rocky Mountain Spotted Fever (RMSF) and ehrlichiosis. These infections are also commonly treated with Doxycycline.
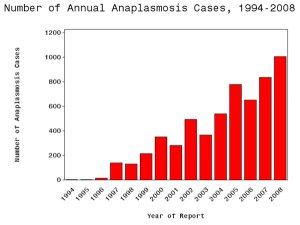
7. The number of cases of Anaplasmosis reported to the CDC has increased steadily since 1996. You can attribute this to climate change or not, but the trend suggests that this disease will be an increasingly more common problem in the future.
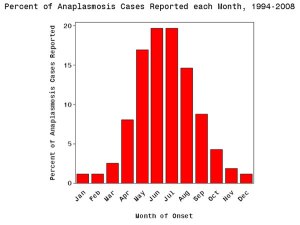
8. More than half of Anaplasmosis cases are reported in the spring and summer months. This is a no-brainer, since this is when tick populations thrive. To avoid infection, take steps to avoid tick exposure for both you and your pets.